During
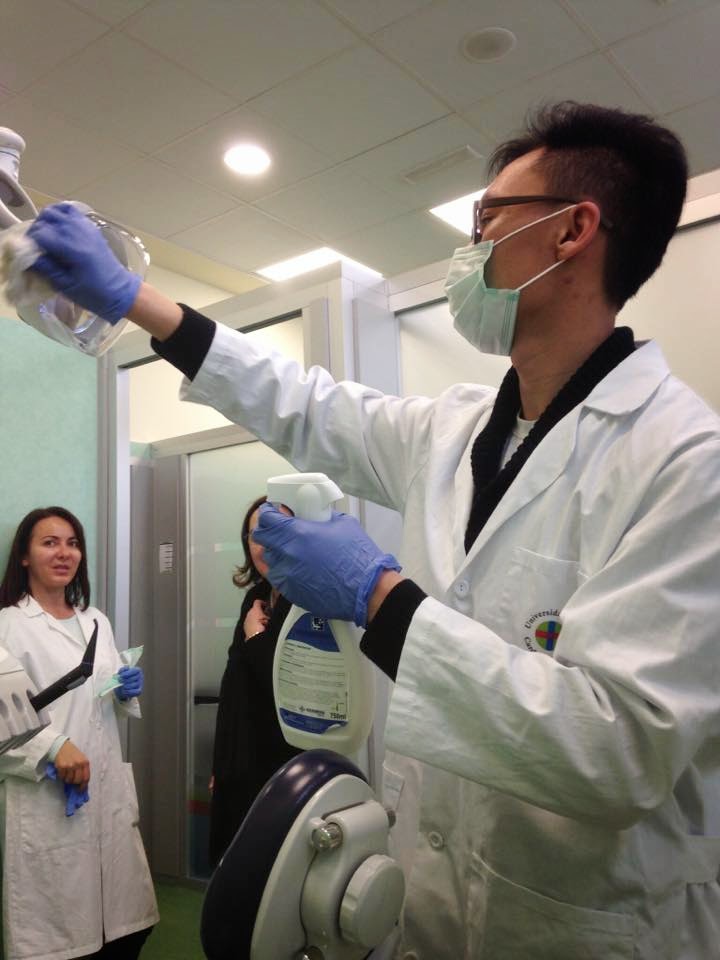
the disinfection and sterilization, we should be noted the nature and characteristics of the method, and
also pay attention to the usable method and external factors about
the disinfection efficacy.
Regardless
of which method we use to disinfection or
sterilization,
the disinfection effect will be affected by many factors, so
if we can control and use the advantage of these factors, it can increase the disinfection
effect. Otherwise, it will lead the disinfection or sterilization to failure.
The main factors are the following points:
1) Sterilize dose:
The
sterilize dose is the basic condition to kill microorganisms,
include the strength and time. If increase the sterilize strength,
also can increase the speed of the sterilization. While decrease the
sterilization time, it also decrease the efficacy. Of
course, if the sterilize strength is lower than the standard, it can’t reach the
sterilize goal even if increase the time.
According to the different types of
biology, so there are the different disinfection effects. In addition, the
number of microbes also affect the result. So before the disinfection, we
should be noted the types and quantities of microbes contamination. In general, the microbial
resistance is stronger or more serious pollution, then the disinfection is also
more difficult.
3) PH value:
Changing
the PH value can affect the results of some sterilizations. One side, the disinfectant will be impacted by the PH value, it result of
increased or decreased the disinfectant activity. On the other hand,
the PH value will impact the microorganism.
4) Antagonism:
For the chemical
disinfection, pay attention to the interference about the antagonistic substances. For example, the quaternaries
effects will be neutralized by the soap or anionic detergents.
And acidic or alkaline disinfectant will be neutralized by the alkaline or
acidic substances, then decrease the disinfect efficacy.
5) Penetration:
When
the instruments are disinfected, the bactericidal factors must be applied to
the microorganism itself directly. Otherwise, it won’t have the bactericidal
effect. For example, UV disinfection effect only can apply
the microorganisms on the surface and shallow liquid, a piece of paper can
reduce 95% the bactericidal effect.